For those of your that may not know, Friday, March 20 was Match Day - the much-anticipated day in which medical students find out where they will do their residency training. For those that may not be in medicine, the path to an MD (medical doctor) degree includes (typically) - 4 years of college, then 4 years of medical school, and then 3-7 years of residency training, depending on what field you decide to pursue.
I am fortunate to be the Associate Program Director for a residency track called the San Francisco General Primary Care program, or SFPC, which is a track within the University of California, San Francisco Internal Medicine residency program. Every year we recruit eight outstanding individuals that exhibit a true commitment to primary care for under-served populations.
Given the leadership roles that our graduates go on to play in caring for vulnerable populations, it gives me great privilege to introduce the newest 8!

Chloe Ciccariello
Chloe is finishing medical school at Mt. Sinai's Icahn School of Medicine. She worked previously as a peer educator, and elaborated on those skills while at Mt. Sinai taking on several leadership positions within the East Harlem Health Outreach Partnership (EHHOP) Clinic. She has also been involved in Primary Care Progress, working towards the goal of having more trainees pursue careers in primary care.
Matt Hickey
Matt is completing medical school at the University of California, San Francisco. He has a strong, long-standing interest in global health and HIV care, most recently working on a project about engaging social networks to aid in HIV treatment. He has also worked on decreasing conflict of interest among academic educators, and education programs for youth.
Ashley McMullen
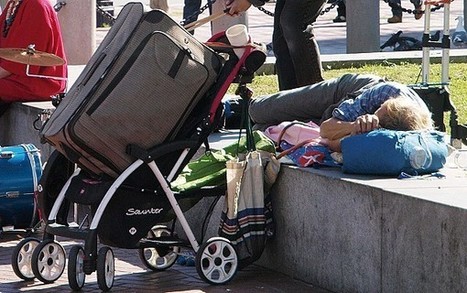
Ashley will be coming from the University of Texas, Houston School of Medicine. She has significant experience in basic science research on tuberculosis, but has developed increasing interest in HIV primary care, working with homeless adults, and advocacy. She has also developed educational opportunities for peers on the topics of street medicine and HIV care.
Alicia Morehead-Gee
Alicia is currently enrolled at the University of California, Los Angeles (UCLA) Drew School of Medicine. Alicia has researched several underserved populations, including HIV-positive adults in South Los Angeles suffering from mental illness and rural Ghanaians. She also has served in leadership roles with the Student National Medical Association (SNMA) and has consistently worked on mentorship and pipeline programs for youth.
Kenny Pettersen
Kenny is finishing medical school at the University of California, San Francisco. Kenny has been a leader in UCSF's student-run Homeless Clinic and has established several programs and performed research in Haiti. He is particularly interested in the role of informational technology in aiding chronic disease management abroad.
Arjun Suri
Arjun will be graduating medical school from Harvard. He has extensive experience working abroad - most recently in Cuba to understand primary care and social medicine training, but also in Peru related to community-driven approaches to quality improvement, and India studying neonatal and maternal health. He is also very interested in systems improvements within urban, public hospitals.
Emily Thomas
Emily is completing medical school at Yale University. She has been particularly interested in studying incarcerated populations and characterizing the health disparities that exist among these individuals. She has also been involved in the student-run free clinic (HAVEN) and supporting fellow students to participate in service activities while at Yale.
Jessica Wang
Jessica is finishing medical school at Yale University, as well. She is interested in improving patient safety by decreasing medication errors. She has also been an active leader in several student-run free clinics at Yale (HAVEN, Neighborhood Health Project). She aims to be a provider and educator in the service of vulnerable patients.
We feel incredibly fortunate to have this group joining our community - Congratulations and Welcome!!